Stroke and Strategic Design
When we looked at the current system for stroke care, we identified two fundamental problems: It is set up to deliver a standard range of care for individual needs and it does so within a fragmented delivery system that varies by region, city, hospital and physician. All of these fragmented activities occur in separate realms driven by their own internal logics. Strategic design is a critical new perspective for stroke care. Current care improvement efforts focus on policy or on process improvement. Without a strategic component, even excellent tactical approaches may simply make poorly conceived care principles more efficient.
Approach
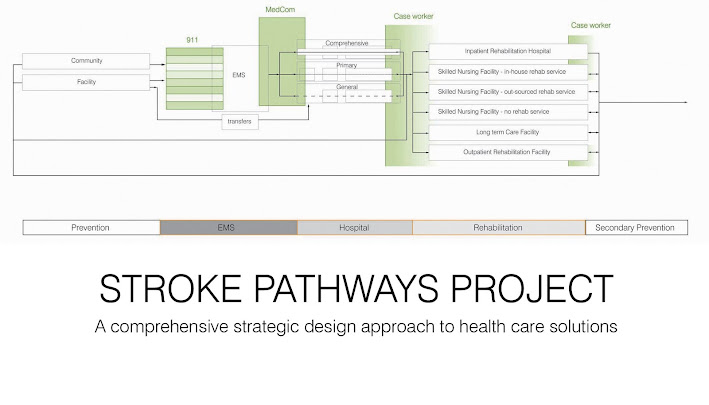
- A full care cycle approach to care-innovations (prevention, acute therapy, long-term needs)
- A systems approach to care delivery, focused on strategic improvements
- A design-centric approach to problem solving
Objectives
Improved patient outcomes (mortality, morbidity, quality of life) at lower costs
Products
Our work delivered the following
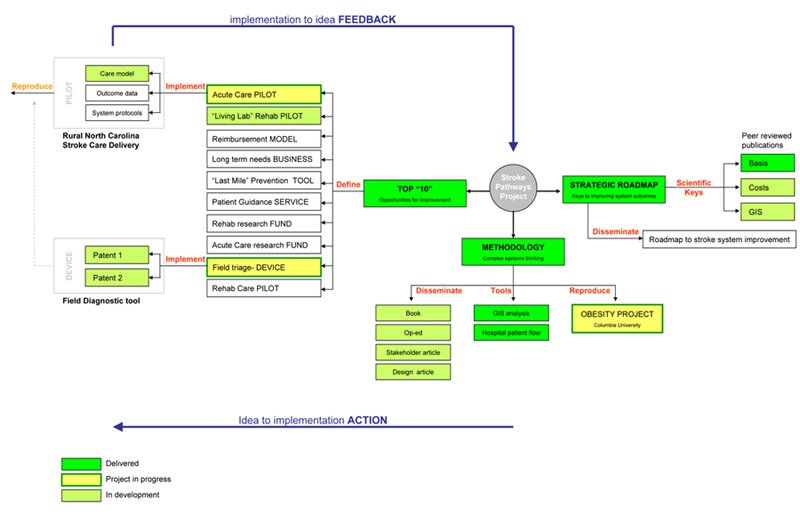
1. A methodology for looking at complex systems
2. A strategic roadmap to improving outcomes at lower costs
3. Defining the “top 10” areas of opportunity for improvement
and we are currently developing
4. Pilots to demonstrate effective improvement
5. A methodology defining the science of implementation